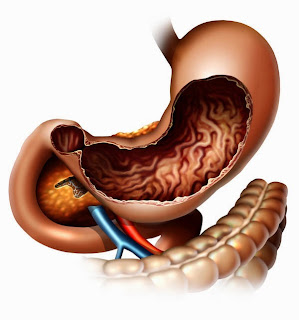
Gastroparesis is a disease that affects the muscles, or the
nerves controlling muscles of the stomach. It results in improper grinding of
food and delayed emptying of the stomach. In a normal person, the vagus nerve
controls the muscles of the stomach which break down the food and move it
further into the intestines by contracting. Any damage to the vagus nerve
whether by injury or illness, will result in disruption of this function. The
most common disease considered responsible for gastroparesis by nerve damage is
diabetes mellitus. The second most common cause is idiopathic; no such reason
can be found and it is termed as idiopathic gastroparesis. An example of the
disease causing gastroparesis due to damage to stomach muscles is Scleroderma.
In some cases, the problem is neither in the muscles not in the nerves; it is
simply due to nerve reflex e.g. when there is pancreatitis. Apart from these,
an imbalance in the levels of minerals (e.g. calcium, potassium etc) in the
blood, and thyroid disease can also be responsible for causing gastroparesis.
Gastroparesis primarily presents with nausea and vomiting
which mainly occurs after meals but can also be due to gastric secretions in some
severe cases. These symptoms are followed by bloating, abdominal pain,
abdominal distention, early satiety (patient feels full on eating small amounts
of food), and weight loss. Improper or reduced food intake further leads to
nutritional deficiencies.
A diagnosis, as in most diseases, is established through a
thorough medical history and physical examinations, blood tests. In this case,
there is a need to rule out structural problems or blockage in the GI tract.
This is done through various tests including upper gastrointestinal endoscopy,
upper GI series, ultrasound, gastric emptying scintipraphy, smart pill (a small
electronic device that is swallowed and then moves around the GI tract and
records information about the time taken for food to pass through the tract),
breath test (radioactive material is ingested and breath samples are taken at
regular intervals to calculate the emptying rate of the stomach). A new study
known as antro-duodenal motility study has emerged that can measure the
pressure generated by the contractions of the stomach and intestinal muscles.
It is however still experimental and reserved for selected case. Another
experimental study called electrogastrogram that works on same principle as EKG
and records the signals that travel through the muscles of the stomach.
Gastroparesis
treatment mainly includes diet, medication and procedures to help emptying
of the stomach. The diet plan is based on foods that are easily emptied from
the stomach; soft, liquid diet. The food should also be low in fiber and should
mostly be eaten early during the day. The medications are given to treat the
underlying conditions such as diabetes mellitus.
Medication to relieve nausea, vomiting and abdominal pain
include promotility drugs (metoclopromide, domperidone, etc), anti-nausea drugs
(prochlorperazine, promethazine, etc), medical marijuana (marinol), serotonin
antagonists (ondansetron), and anticholinergics (scopolamine).
Drugs for reliving abdominal pain include NSAIDs (ibuprofen,
naproxen, etc), tricyclic antidepressants (amitriptyline), nerve blockers
(gabapentin), narcotics (tramadol, fentanyl, etc). Some drugs such as
cisapride, domperidone, metoclopromide, and erythromycin are used to stimulate
the contractions in the muscles of the stomach. As the stomach emptying is
affected, liquid medications are preferred over oral as they are more effective
in this condition.
A new method called electrical pacing is used to treat
severe cases of gastroparesis. A pacemaker for the stomach is placed
laproscopically and then generates impulses. Surgery can also be performed to
facilitate emptying by creating a larger opening between the stomach and
intestines. Sometimes, the entire stomach may be removed. However, surgery
should be the last option of treatment.
Patients of gastroparesis suffer from malnutrition and
dehydration which can be managed by IV fluids and replenishing of electrolytes.
This involves methods such as IV total parenteral nutrition (TPN) and enteral
nutrition. Enteral nutrition is preferred over TPN and can be done via naso-jejunal
tubes or jejunostomy tubes. Treatment with
botulinum toxin may be effective but is currently under study.
Clinical research is being conducted at National Institute
of Diabetes and Digestive and Kidney Disease (NIDDK), for new medications or
surgical methods that can cure gastroparesis more effectively and safely. More
information can be found at cancercarevilla.blogspot.com.
















.png)





